Content note: Some of the links throughout this post include graphic images of surgery. Click with caution!
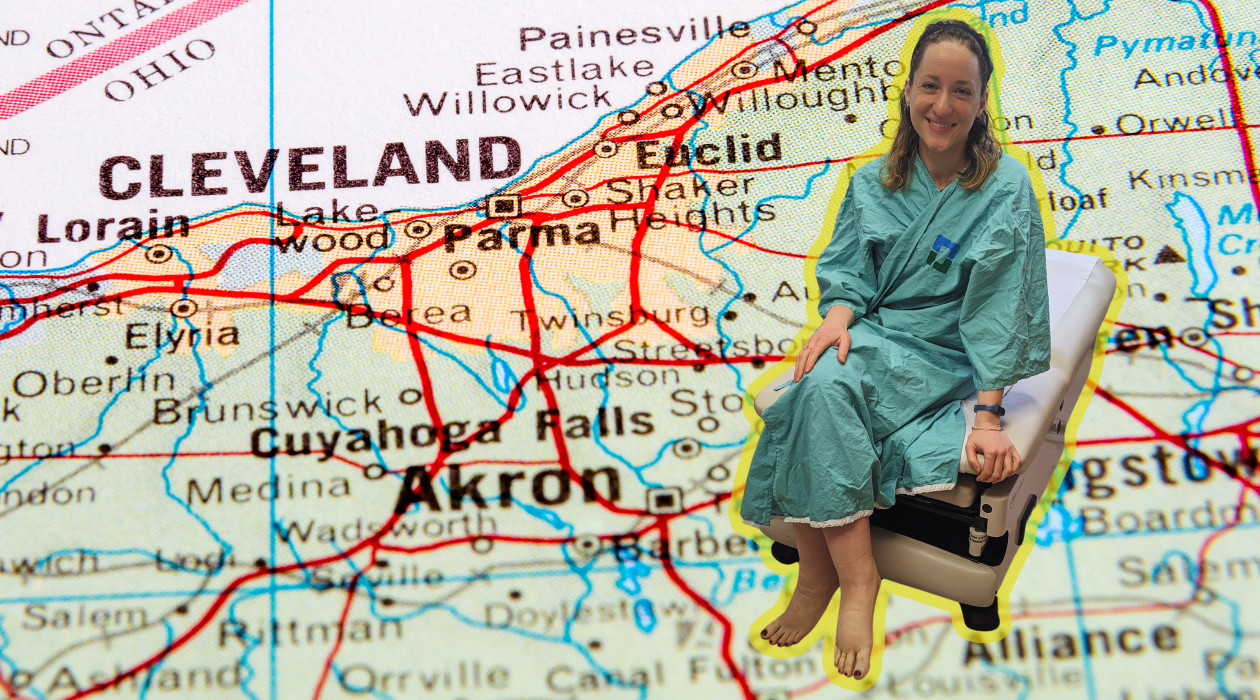
At the end of March, I was somewhere I never expected I’d be: Sitting in an exam room at the Cleveland Clinic’s Plastic and Reconstructive Surgery Department, wearing a paper gown. In the chair beside me sat my twin sister, pen and notebook at the ready.
We were waiting to be seen by Dr. Wei F. Chen to talk about surgery for my lymphedema.
We had flown in the day before, but my journey to Cleveland actually started five years prior, in Boston.
Picture it: Boston, 2019
While at the National Lymphedema Network Conference in 2019 to present my talk on “The Language of Lymphedema,” I volunteered to undergo an infrared fluoroscopy onstage as part of a live demonstration.
This imaging technique involves a subcutaneous injection of the medical dye indocyanine green (ICG), which is taken up by the lymphatic system. By using an infrared camera, you’re then able to assess lymphatic function (or lack thereof) by seeing where the dye travels.
From what I understood prior to the fluoroscopy, my right leg was my affected leg and my left, although occasionally swollen, was my “good” limb. The demonstration, however, suggested differently.
During the fluoroscopy, my right leg was aglow with the green dye, indicating dermal backflow (the leaking of lymphatic fluid into surrounding tissue). The left leg, however, showed no glow at all aside from the injection sites — the dye hadn’t moved. This could be interpreted as lymphatic hypoplasia, which is the underdevelopment of lymphatic vessels.
My results were described to me as showing a classic primary disease pattern, which makes sense — I’ve already been diagnosed with primary lymphedema — however the lack of functioning lymphatics in my left leg threw me for a loop. Obviously this infrared fluoroscopy demonstration wasn’t a definitive imaging of my lymphatics, but it was still the first peek into the workings of my lymphatic system that I’d ever had.
After the demonstration, I ran into Dr. Chen, and we talked about what we saw. He asked if I had ever considered surgery, because I could probably be a candidate for something like lymphovenous anastomosis, a microsurgery where lymphatic vessels are directly connected to nearby veins to aid in draining excess lymph fluid.
I never considered myself a candidate for surgery before. I thought my swelling wasn’t “bad enough” to justify surgical intervention and that wearing my garment was enough to manage my lymphedema, but after that conversation, I couldn’t stop thinking about it.
A couple weeks after the conference, during an appointment at my lymphedema clinic, I told my doctor about the fluoroscopy and its findings and asked if he thought I should pursue surgery.
He shook his head “no”: My lymphedema was mild and well-managed enough that surgery wasn’t necessary, he said. It wouldn’t do anything.
When he left the room, one of the lymphedema therapists hung back and asked to speak candidly with me. “If it were me, and I had the chance to alleviate a progressive condition like this,” she said, gesturing at my leg. “I’d do it.”
I ran into Dr. Chen a couple more times at conferences over the years, and during our small talk he’d ask if I gave any more thought to surgery. Every time, I’d say no. But my leg was getting heavier over the years, despite my best efforts to keep the swelling down. Finally, at the 2023 NLN Conference, I told him I was ready, and he encouraged me to give his office a call to schedule a consult.
My Consult at Cleveland Clinic
Fast forward again to March 2024 in Cleveland, Ohio.
It was the night before my consult. My sister and I were eating room service pizza with Nasreen Starner, one of my lymphedema therapist friends who has a clinic in nearby Westlake. After catching up, she offered to perform manual lymphatic drainage on my leg.
It was heavenly, especially after having traveled earlier that day. Not only did she work the front of my leg, but the back, too, prompting what could best be described as a Seinfeldian exchange, if George Costanza had lymphedema:
“I’ve never been flipped before!” I exclaimed, after Nasreen had me roll onto my stomach so she could massage the backs of my calves and thighs.
“You’ve never been flipped?!” she said, in equal disbelief.
“Never flipped!”
The back of the leg, she explained, has a different drainage pattern, so it’s important to massage both front and back of the body for proper clearing. As she worked her magic on my swelling, she talked me through what to expect at the appointment, easing both my mind and my lymphatic system. (Thanks, Nasreen!!)



The next morning, my sister and I made our way to the Plastic and Reconstructive Surgery Department and got checked in at the reception desk. After about an hour wait, we were finally called back.
I was seen first by a couple nurses, who asked general intake questions about my medical history and lymphedema, then had photos taken of my legs to submit to insurance. Then a lymphatic supermicrosurgery fellow came in and examined my legs, asked a lot of questions, and answered even more of my own, as my sister dutifully jotted down notes. Dr. Chen came in not long after, performing his own examination and talking me through his recommendations and next steps.
All told, we were there for about five hours, although a lot of that time was spent waiting in between assessments. The whole appointment was information overload, all the more reason I was grateful to have my sister with me to help absorb and process it all.
My Exam and Assessment
Dr. Chen observed that my right leg, ankle, and foot were visibly larger than my left, complete with fibrotic lipodystrophy (meaning an abnormal distribution of fat).
My left leg, ankle, and foot also presented with lipodystrophy, albeit milder, and with no significant fibrosis. The lack of skin elasticity and the absence of a visible shin made it clear that my left leg — the one I always considered my “good leg” — was undoubtedly affected. This was something I suspected for a while now, but my heart still did a panicky jump at the confirmation.
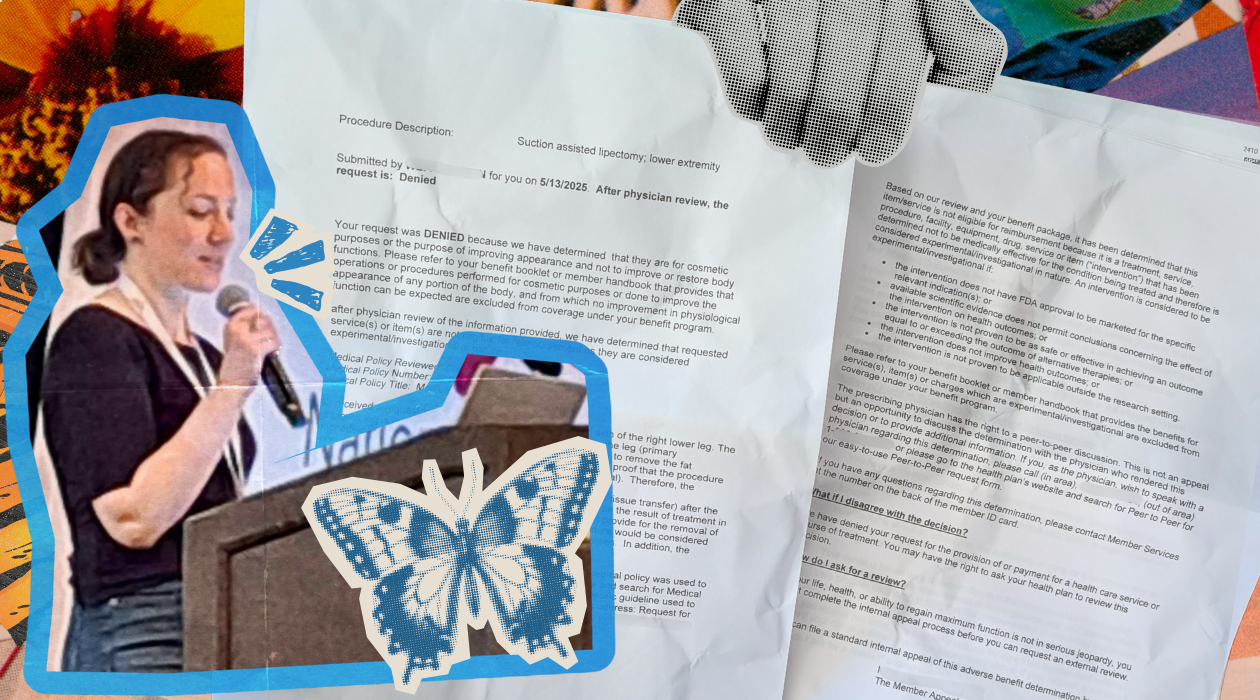
Neither of my legs had pitting, which means my swelling is primarily made up of excess adipose tissue, or fat, rather than lymph fluid. Because my lymphedema is solid-predominant rather than fluid-predominant, Dr. Chen recommended I undergo a suction-assisted protein lipectomy (SAPL) as well as a minimally invasive tissue excision with possible redundant skin excision (MITESE). Or, in more basic terms, liposuction and excess skin removal.
This all would be done on my right lower leg, ankle, and foot, but my left leg will likely benefit as well: When it comes to primary lymphedema, Dr. Chen explained, there’s no such thing as “localized lymphedema,” meaning it’s systemic; surgery would lead to global improvement.
This includes the brain’s lymphatic system, too, as new evidence has shown recipients of lymphatic supermicrosurgery reporting improved cognition following their lymphedema surgeries. (Awesome news for me and my brain fog.)
Depending on my outcomes, I may or may not get the same done on my left leg. I also may or may not undergo supermicrosurgical lymphaticovenular anastomosis (LVA) in a hybrid approach to further reconstruct and improve my lymphatic function. With all the gunk removed after the SAPL, an LVA would stand a much better chance.

Why now?
Up until a few months ago, I didn’t fully understand the long-term effects of lymphedema. Like, I knew it was a progressive condition and my leg could worsen in volume overtime, but I had no idea what was happening underneath my skin, the physiological changes wrought by the prolonged accumulation of lymph fluid, adipose tissue, and fibrosis.
Things have progressed more than I thought in both my legs. If I wait any longer to do this, things will only get worse for my lymphedema. In fact, Dr. Chen pointed out that my recent episode of cellulitis indicated that my lymphatic system was struggling more than it had before, especially with that being my first infection.
He considered the surgery time-sensitive, meaning the sooner we proceed with surgery, the less technically challenging it is expected to be, and the more successful.
I thought again about what my lymphedema therapist said five years before, about taking the chance to help myself.
It’s time to do this.
It’s time I help myself.
Why Dr. Chen?
There’s a number of talented and accomplished surgeons out there. Living in Baltimore, it would seem like Johns Hopkins would be an obvious choice, or perhaps someone at nearby Penn Medicine.
But I only had eyes for Dr. Chen. Not only am I most familiar with him and his approach to microsurgery, but I appreciate how engaged he is in the world of lymphedema and lymphatics. He shows up for the community, whether it’s actively attending and presenting at conferences, conducting research, or doing virtual webinars for patient groups, and that means a lot to me as a person living with lymphatic disease.
Like most lymphedema patients, I’ve had too many encounters with medical professionals unfamiliar with the lymphatic system or lymphedema, and even more who were unwilling to learn. To me, there’s a big difference between a surgeon who performs lymphatic microsurgery and a surgeon who truly understands it. I’ve had the pleasure of listening to a few presentations by Dr. Chen over the years, and to hear his knowledge of and respect for the lymphatic system is really inspiring.
The good thing is that there are a number of passionate surgeons like Dr. Chen doing lymphedema surgeries. If you’re considering surgical treatment, I encourage you to do your research to find a surgeon that would be the best fit for you and your needs. Some great places to start are the Lymphatic Education & Research Network’s Centers of Excellence directory or posting in virtual support groups to hear others’ experiences.
What’s next?
The months following the consult were spent processing it all. I was excited but a little nervous, my head swarming with all sorts of thoughts and feelings. I even avoided writing this post because condensing the experience into words felt a bit overwhelming.
But it’s official: My insurance approved the procedure, and I’m officially scheduled for surgery this November.
To prepare, I’ll be working with my lymphedema clinic in the weeks ahead of surgery to do a short course of complete decongestive therapy. This will help “prime the pump” for my lymphatic system, so to speak, so I can have better surgical outcomes.
I’ll also undergo diagnostic testing at Cleveland Clinic a couple days before the actual procedure. This will include bioimpedance, a 3D volume scan, and an indocyanine green lymphography of all four extremities to visualize and assess my lymphatic function.
I feel optimistic: Whether it’s SAPL, LVA, or vascularized lymph node transfer surgery, I know a lot of people in the community who’ve successfully undergone surgeries to treat their lymphedema. And I’m fully aware that, although Dr. Chen is vocal about surgery’s potential to offer a clinical cure for lymphedema, I will still need to wear my flat-knit compression garments, use my pneumatic compression pump, and continue all the other things I do every day to manage my lymphedema. I may even need to get another surgery down the road.
After getting SAPL, my underlying lymphatic dysfunction will still be there. But with all that disease-compromised tissue and fatty deposits removed, my lymphatic function will improve, the volume will reduce, and my symptoms will be that much easier to manage. My leg won’t feel so heavy and uncomfortable, and my brain fog may even clear up a little, too.
My quality of life — and the quality of my lymphie life — is about to get so much better.
So stay tuned and #StayElevated as my surgical journey continues!